Canada is widely regarded as a country with a universal and publicly funded healthcare system that provides access to quality care for all citizens. However, a harsh reality lies behind this idealized picture. In fact, its an open secret that in 2024, Canada’s healthcare crisis is growing while it struggles to meet the increasing demands and expectations of an aging and growing population.

The Canadian healthcare system is facing a crisis of understaffing, over-demand, and poor quality of care that threatens the health and well-being of Canadians. In this article we will examine the causes and consequences of this crisis—as well as some potential solutions to address the challenges. The article aims to raise awareness and spark a dialogue on how to solve Canada’s healthcare crisis and where Canadians can go to get better care if they require it.
Under-staffing Levels Contribute to Canada’s Healthcare Crisis

The main cause of Canada’s healthcare crisis is the chronic understaffing of hospitals across the country. Under-staffing means that healthcare workers have to deal with heavier workloads, longer shifts, and fewer resources. A recent poll by the Ontario Council of Hospital Unions (OCHU) found that:
- 69% of healthcare workers feel that there is an inadequate number of staff to provide high-quality care
- 40% of hospital workers are considering quitting their jobs due to the unbearable working conditions
- 71% of racialized workers report they are subject to harassment or abuse because of their race or appearance
- 49% of all categories of hospital workers experience sexual harassment, and 36% experience sexual assault
Is it any wonder that burnout and resignations are now endemic among those we rely upon most during health emergencies?
Perhaps it’s time our leaders took a brief hiatus from political posturing and actually listened to those on the frontlines of Canada’s healthcare crisis.
Unless steps are immediately taken to bolster staffing levels, our hospitals may soon face a collapse of epic proportions.
But at least we can always comfort ourselves that other critical issues like tax cuts stay firmly at the top of the agenda. The well-being of Canadians and our healthcare workers seems a lower priority for those who can only see as far as the next election cycle. It appears the system will continue to lurch from one understaffing emergency to the next until we demand better.
Root Causes of Under-staffing
The shortage of healthcare workers in Canada is not a new phenomenon but a result of decades of neglect and underinvestment in the health workforce. The root causes of this shortage are complex and interrelated, but they can be summarized as follows: low wages, precarious employment conditions, and government policies.
1). Low wages
Despite the vital role that healthcare workers play in the health system, many of them are paid poorly compared with other occupations.
For example, the average hourly wage of personal support workers or care aides in Canada was $19.02 in 2023, lower than the national average of $28.00 for all occupations. Low wages discourage people from joining or staying in the healthcare profession, especially when the cost of living and education are increasing.
3). Government policies
Government policies have also contributed to the shortage of healthcare workers by failing to address the current and future needs of the health workforce. For example, government funding for health care has not kept pace with the demand for services, resulting in cuts, closures, and rationing of care. Government policies have also restricted the immigration and integration of internationally educated health professionals, who could help fill the gaps in the workforce.
2). Precarious employment conditions
Many healthcare workers face precarious employment conditions, such as temporary, part-time, or casual contracts, lack of benefits, and limited opportunities for career advancement.
These conditions increase the uncertainty and instability of their work, as well as their exposure to health and safety risks. For instance, a study found that precarious work was associated with higher levels of job stress and lower levels of health-related quality of life among nurses.
4). COVID-19 pandemic
The COVID-19 pandemic has exacerbated the situation by increasing the workload, stress, and burnout of healthcare workers.
The pandemic has exposed the vulnerabilities and weaknesses of the health system. Healthcare workers have faced unprecedented challenges, such as shortages of personal protective equipment, increased exposure to infection, increased violence and harassment, and increased moral distress.
These are the root causes of Canada’s healthcare crisis, which require urgent and comprehensive solutions. Otherwise, the health and well-being of healthcare workers and the public will continue to suffer.
Canada’s Expanding Population and it’s Future Consequences
Another factor that is contributing to Canada’s healthcare crisis is the expanding and aging population, which puts more pressure on the already overwhelmed system.
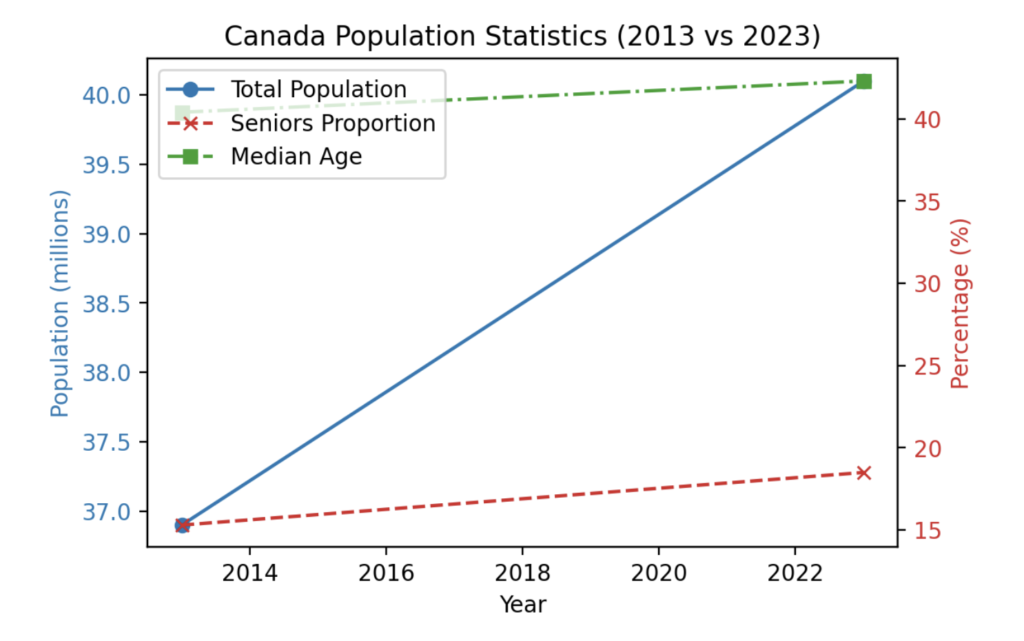
Canada’s population has grown by 8.6% from 2013 to 2023, reaching 40.1 million people. Most of this growth is due to immigration, which accounts for 96% of the population increase.
Moreover, Canada’s population is aging rapidly, as the proportion of seniors aged 65 and over increased from 15.3% in 2013 to 18.5% in 2023. This trend is expected to continue, as the median age of Canadians rose from 40.4 years in 2013 to 42.3 years in 2023.
An expanding and aging population means more demand for health services, especially for chronic and complex conditions. According to Statistics Canada, 81.2% of Canadians aged 65 and over reported having at least one chronic condition in 2023, compared with 56.7% of those aged 12 to 64.
Chronic conditions such as diabetes, heart disease, and cancer are associated with higher healthcare utilization and costs, as well as lower quality of life and increased mortality. Furthermore, an aging population also requires more long-term care, home care, and palliative care, which are often underfunded and undersupplied in the current system
Clearly, the expanding and aging population poses a significant challenge for the Canadian healthcare system, which requires urgent and comprehensive solutions. Otherwise, the health and well-being of Canadians will continue to deteriorate and Canada’s healthcare crisis will continue to grow.
Consequences of Understaffing & Expanding Population – Increased Wait Times
The current system is unable to meet the demand for services, resulting in long wait times, access barriers, and poor outcomes. For example, in 2023, the median wait time for medically necessary treatment in Canada was 27.7 weeks, the longest ever recorded.
Long wait times can have serious consequences for patients, such as increased pain, disability, and risk of complications or death.
In fact, a recent report revealed that more than 17,000 Canadians died while waiting for surgery or diagnostic scans in 2022-23, but that number could be significantly higher. This is a shocking and unacceptable outcome for a country that prides itself on its universal healthcare system.
The report, which was based on freedom of information requests made to 33 healthcare bodies across the country, found that patients waited anywhere from less than a week to nearly 11 years for their procedures. Some of the examples of people who died waiting and the consequences of delays are:
- A 64-year-old man in Ontario died of a heart attack while waiting ten months for a coronary artery bypass graft.
- A 25-year-old man in Saskatchewan died of a brain tumor while waiting four months for an MRI.
- A 72-year-old man in Alberta died of sepsis while waiting six months for a colonoscopy.
- A 32-year-old woman in Manitoba died of cervical cancer while waiting seven months for a hysterectomy.
The report also estimated that the total number of procedures for which people were waiting in 2021 was 1,425,517, which means that 3.7% of Canadians were waiting for treatment. The proportion of the population waiting for treatment varied from a low of 2.96% in Ontario to a high of 10.76% in Nova Scotia.
The increase in wait times for surgeries and procedures is not only a result of the COVID-19 pandemic, which disrupted the delivery of non-urgent care, but also a reflection of the chronic under-staffing of hospitals, which limits the availability and capacity of operating rooms, beds, and equipment. Moreover, the increase in wait times also affects the demand and supply of
health care, as longer waits can lead to more complications, deterioration, and referrals, which in turn can increase the need for more resources and staff.
The increase in wait times for surgeries and procedures is a serious and urgent problem that needs to be addressed, as it violates the right to timely and appropriate health care, as well as the right to life, of Canadians. The question is, will the government and the hospitals take action against Canada’s healthcare crisis to reduce the wait times, or will they continue to let patients suffer and die?
Potential Solutions
Although it will be tough, Canada’s healthcare crisis is not irreversible and with some dedication it can be solved.

One of the most obvious solutions is to increase the funding for health care, both from the federal and provincial governments. Increased funding could help address the gaps in infrastructure, equipment, and supplies, as well as support the recruitment and retention of healthcare workers. Increased funding could also enable more investment in prevention, promotion, and primary care, which could reduce the demand for costly and complex care.
However, simply increasing funding alone is not enough, as it does not guarantee efficiency, effectiveness, or equity. Perhaps we could learn from some overseas examples of how to actually spend those funds effectively.
- Germany – Investing in Education: In Germany, the government increased nursing school enrollment by 15% and offered generous tuition subsidies. What a novel idea – ensuring an educated workforce for the future! Meanwhile, in Canada, we can’t even keep up with annual attrition rates.
- United Kingdom – Improving Working Conditions: The National Health Service in the UK implemented initiatives like flexible scheduling, increased mentorship for new nurses, and bonuses for working in understaffed areas. While we’ve all seen how well-managed the NHS is, this shows even simple measures can help retention. But heaven forbid we treat healthcare staff like valued members of the team!
- New Zealand – Long-Term Planning: New Zealand’s Ministry of Health conducts annual workforce surveys and uses the data to project needs over the next decade. They then adjust education targets proactively instead of constantly playing catch up. It must be nice living in a country where the government plans beyond the next election cycle.
You can see that just throwing a few extra pennies at the problem while maintaining the status quo will not come close to resolving Canada’s healthcare crisis. Bold reforms and long-term strategies are desperately needed.
Wrapping up
Canada’s healthcare crisis demands urgent attention and comprehensive solutions. Under-staffing, worsened by low wages and precarious conditions, has led to alarming statistics, burnout, and an exodus of healthcare professionals. The expanding and aging population further strains the system, resulting in record-long wait times and, shockingly, preventable deaths.
Immediate action, including increased funding, policy reforms, and global best practices, is imperative. The status quo, marked by political posturing and insufficient measures, risks the collapse of a once-praised healthcare model. The well-being of Canadians and healthcare workers should be prioritized over short-term gains, urging a collective commitment to address this critical issue before irreparable damage occurs.
Looking to leave Canada?
Take the country quiz to see where you belong!


Leave a Reply